Deep circumflex iliac artery (DCIA) bone flap
Anatomic considerations
The deep circumflex iliac artery bone flap provides a large concave segment of bone suitable for reconstruction of the upper extremity, lower extremity and mandible. Although the fibula has often replaced the DCIA when bone reconstruction is necessary, especially in the mandible, the DCIA provides a large segment of cancellous bone up to 15 centimeters long and 6 centimeters wide. The fibula, in contrast, supplies only cortical bone. In addition, when the peroneal artery inflow is not adequate, or the lower extremities have been injured, the DCIA is an excellent choice when a large block of bone is necessary in lieu of the fibula.
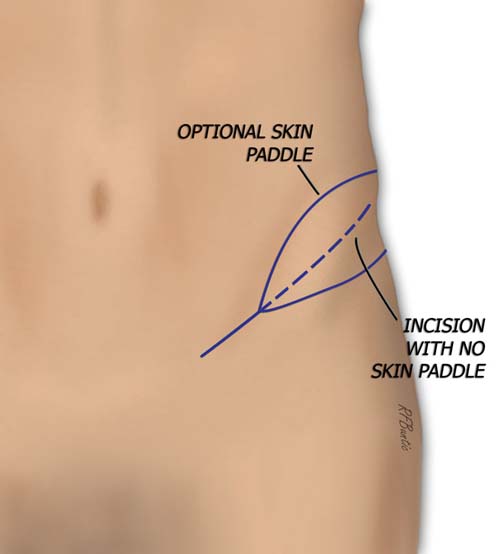
The flap can be harvested with or without a skin paddle. The skin paddle can make the flap quite thick however, often making inset difficult. We prefer a second flap, such as the groin flap, which can be harvested in the same field, often with the same vascular trunk to the groin flap and the DCIA flap. Separating the groin from the DCIA flap provides an independent skin paddle that is thinner and easier to inset. The disadvantage is the frequent separate origin of the DCIA and groin pedicles and the subsequent need for two more microvascular anastomoses in one setting.
Anatomy
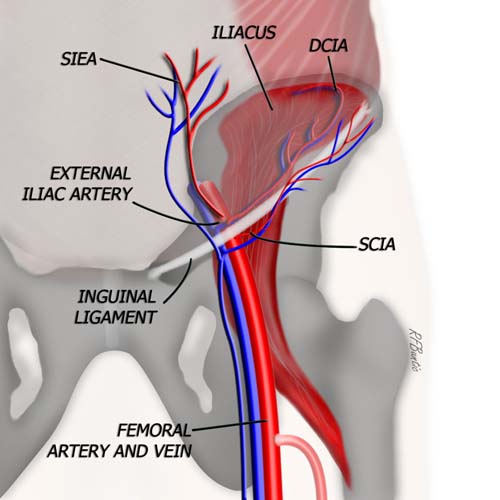
Vascular anatomy of the DCIA flap. The SCIA and DCIA may have a common origin from the external iliac/superficial femoral artery.
SCIA: Superficial circumflex iliac artery.
DCIA: Deep circumflex iliac artery.
SIEA: Superficial inferior epigastric artery.
The DCIA flap relies on inflow from the vessels originating near the junction of the external iliac artery and the femoral artery at the inguinal ligament. The DCIA may take origin from the external iliac artery alone, or with a common trunk that provides both the DCIA and the SCIA (superficial circumflex iliac artery). Slightly more cranial to these vessels and originating on the external iliac artery, is the origin of the superficial inferior epigastric artery (SIEA). The vein to the DCIA empties into the saphenous vein or a tributary, and then flows into the femoral vein.
Operative Procedure
The patient is prepped and draped supine, with a well padded bump under the hip to elevate and externally rotate the donor area. The iliac crest surface from the anterior superior iliac spine, curving posteriorly, is marked for orientation. The femoral vessels in the inguinal crease are palpated and identified. The course of the inguinal ligament is noted and the superficial circumflex iliac artery can be found with a pencil Doppler if desired. If a skin paddle is to be harvested, we find the superficial circumflex vessels so that the skin paddle can be isolated on this pedicle. The incision is marked a finger breadth above and parallel to the inguinal ligament.
After the incision is made, the SCIA and DCIA vessels are identified at or near their origin. Once identified, the DCIA vessels are traced distally toward the anterior superior iliac spine, in the substance of the transversalis fascia. The external and internal oblique muscular fascia is divided superficial to and along the course of the artery and vein. During this course as the surgeon proceeds laterally, the lateral cutaneous nerve of the thigh is encountered. If it can be preserved, it is, if it cannot, then it is divided and repaired before closure.
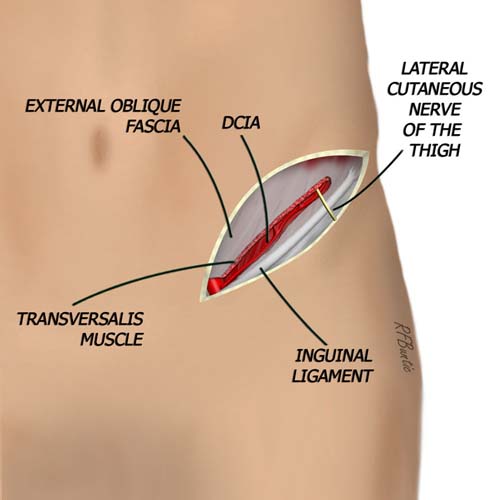
DCIA flap without skin paddle. The vessel is found lateral to the origin and traced distally toward the anterior superior iliac spine.
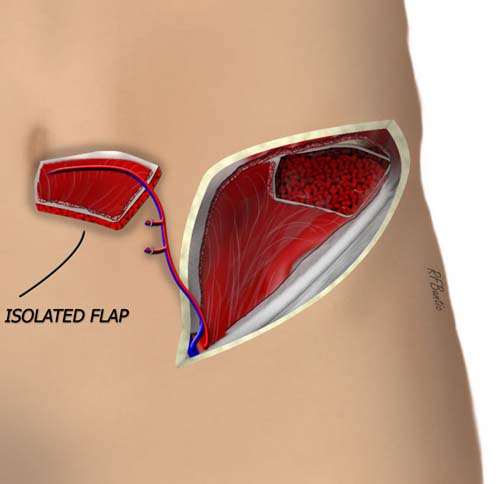
As the dissection proceeds laterally and the iliac crest is encountered, the muscles superficial to the pedicle are divided from the iliac crest insertion, exposing the iliacus muscle and iliac crest. The vessels lie on the surface of the iliacus muscle, guiding the dissection as it proceeds posteriorly. The vessels diverge later into branches that penetrate the iliacus and the overlying transversalis fascia.
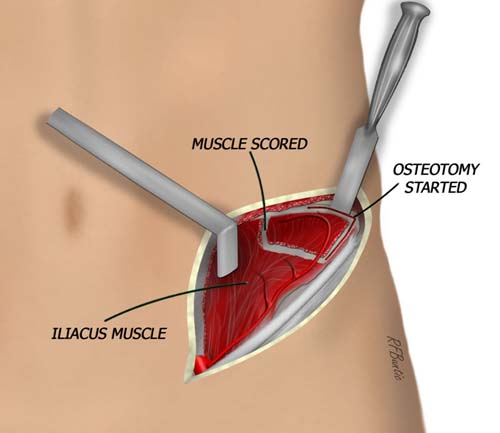
The iliac crest is exposed and the ilacus muscle is scored to circumscribe the area of bone harvest. Full thickness bicortical graft is optional, unicortical bone preserves the contour of the iliac crest.
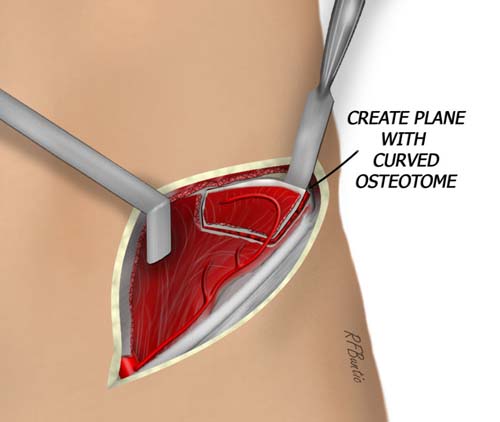
When the appropriate length of iliac crest is isolated, the osteotomies can be performed. We prefer to isolate inner table only and leave the outer table, however, there are times when full thickness iliac crest is required. If full thickness bone is required the external lip of the iliac crest is dissected, detaching muscle from the posterior lip until the bone flap size required is exposed.
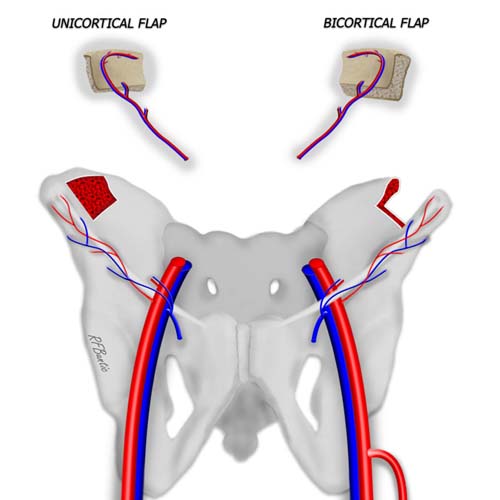
The full thickness bicortical or partial thickness unicortical flap of the iliac crest can be harvested as illustrated.
On the anterior surface of the iliac crest, the cautery is used to score the iliacus muscle and "square off" the area need for osteotomy. We perform the osteotomies with sharp osteotomes, but they can be performed with the oscillating saw as well. If inner table only is necessary, the curved osteotome is used to separate the inner iliac cortical bone from the posterior cortical bone. This is done in the cancellous layer, hugging the posterior cortex as the osteotome is tapped. When the bone flap is isolated, the pedicle is traced with the flap to near it's origin, and divided when the recipient team is ready.
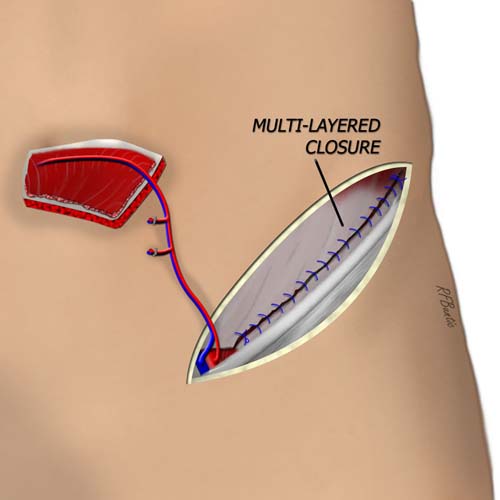
Bleeding bone edges can be treated with bone wax
The closure must be meticulous and in layers. The iliacus muscle is sewn to the internal oblique with large braided suture to seal the pelvic contents from potentially herniating. The external oblique layer is closed with interrupted or large running suture to get a tight seal of the muscular layer over the iliac crest and toward the inguinal ligament. Closure is usually performed over suction drains.
Flap variations
The flap can be harvested with or without a skin paddle. The skin paddle can be harvested on a separate pedicle as a groin flap.