Vascularized Fibula Flap
Anatomic considerations
The reliability of the skin paddle harvested with the fibula flap has been questioned. Strategies to increase reliability have included harvesting a greater length of paddle and septum and trying to predict the location of septal perforators. We have found that using perforator flap techniques and tracing intramuscular perforators when no septal vessels are available, greatly increases reliability of this flap and enhances skin perfusion.
Anatomy
The fibula is a long thin bone that has close proximity to the peroneal artery and venae and can therefore be harvested on a single large pedicle. The length of the bone, consistent blood supply and relative ease of harvest make this donor one of the most useful when osseous reconstruction is required. It has become the workhorse for mandible reconstruction and segmental long bone defects in both the upper and lower extremities.
The head of the fibula does not take part in the knee joint, although it does have an articular surface with the lateral condyle of the tibia. Just distal to the head, the neck is looped by the peroneal nerve. This close relationship with the nerve is significant because any osteotomy in this area can subject the nerve to injury. The shaft of the fibula is palpable laterally, but somewhat protected by the lateral compartment. The shaft has four surfaces, approximating the shape of a square in cross-section. The distal end of the fibula forms the lateral malleolus where the bone articulates medially with the talus. Because the fibula is part of the ankle joint, the distal six centimeters of the fibula are preserved to avoid disruption of the ankle joint. The skin island can be marked on an axis slightly posterior to the axis of the bone. We usually harvest a paddle length close to the entire length of bone we will harvest, to increase the number of perforators and allow for more options to tailor the flap inset. A paddle up to 5 centimeters wide can be closed primarily.
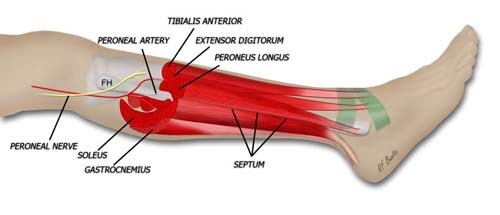
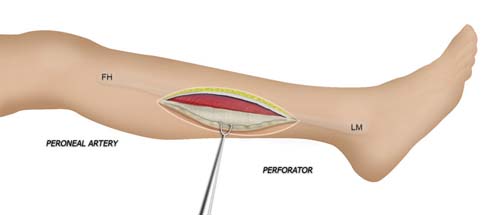
Muscular and vascular anatomy of the lower leg. The peroneal artery supplies the fibular flap and perforators to the overlying skin. It lies deep to the fibula.
Vascular Anatomy
The peroneal artery is closely positioned to the fibula. The artery arises from the tibioperoneal trunk, distal to the takeoff of the anterior tibial artery (seen in the illustration below perforating the interosseous membrane). The peroneal artery sends perforators laterally to the skin of the lower leg, sometimes in a septocutaneous fashion via the lateral intermuscular septum, but often with muscular perforators. The length of the pedicle is usually short, but can be increased substantially by dissecting the peroneal artery and its venae from the fibula and using the distal bone for reconstruction.
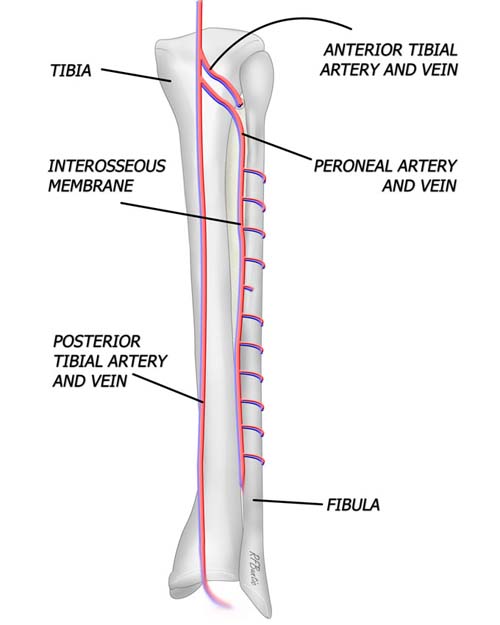
Vascular relationships of the fibula. The peroneal artery leaves the tibio-peroneal trunk just below the take off of the anterior tibial artery. The peroneal artery hugs the fibula deep to its surface and posterior to the interosseus membrane.
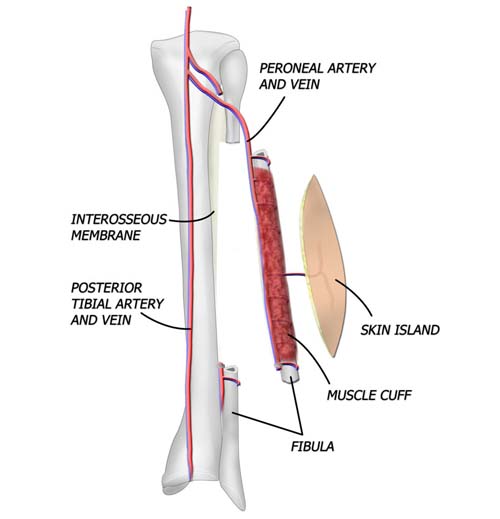
Anatomical relationships of the isolated flap. The bone requires a cuff of muscle approximately 1 to 2 millimeters in thickness be harvested with the flap to protect the vascular inflow to the bone flap. Perforating vessels from the peroneal artery also provide circulation to the skin flap that can be taken with the flap.
Muscle and Cross-Sectional Anatomy
In cross-section , the interosseous membrane is seen in green, spanning from the tibia to the fibula. The lateral intermuscular septum separates the lateral compartment muscles from the soleus. When harvesting the osteocutaneous flap, the septum is harvested in continuity with the paddle of skin and fascia of the lateral leg.
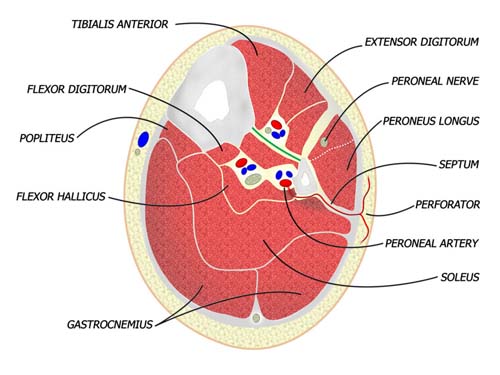
Cross section of the lower leg distal to neck of fibula. The peroneal artery runs deep to the fibula, just posterior to the interosseous membrane.
Fibula Flap Pre-Operative Assessment
Both lower extremities must be evaluated to determine the presence or extent of any disease and to ascertain the pulse status of the patient. The feet are examined for signs of peripheral vascular disease and the anterior and posterior tibial pulses are palpated. Because an intact arch can supply retrograde flow to the major vessels of the foot, it can be helpful to put pressure on the anterior tibial artery when detecting the presence of a posterior tibial pulse and visa-versa. This "modified Allen's test" may detect proximal vessel obstruction masked by an intact foot arch.
The need for preoperative angiography in young, healthy patients with a normal physical examination has been hotly debated. Our tendency has been to obtain preoperative angiograms as a guide. Although rare, we have seen lower extremities with a dominant peroneal artery nourishing the foot and distal anterior and posterior vessels, contraindicating sacrifice of the peroneal artery. MRI or CT angiography can also be used in many circumstances.
Fibula Flap Harvest
The patient is placed in the supine position with a bump under the ipsilateral hip to lessen the need for excessive internal rotation of the lower leg. Alternatively, the lateral decubitus position can be used, with the harvest leg placed up and the patient held in position with a beanbag. A well padded tourniquet is placed on the thigh and the leg from the knee down is prepped and draped. The proximal and distal fibula are marked and the axis of the bone is drawn.
The axis of the skin paddle is drawn at the posterior border of the fibula. The paddle is outlined a few centimeters below the neck of the fibula and 5 to 5 centimeters above the medial malleolus. If less skin paddle is needed, a smaller paddle can be drawn, or the skin can be trimmed after the flap is harvested.
If no skin paddle is needed, the incision is simply made along the axis of the bone, a finger breadth posterior to the fibula. The dissection proceeds to the fibula and the bone is isolated as shown below.
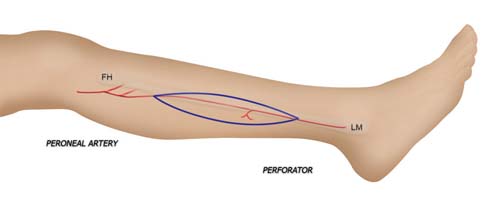
Perforating vessels are identified along the axis of the fibula. The skin paddle incorporates a loud perforator near the midpoint of the shaft of the fibula.
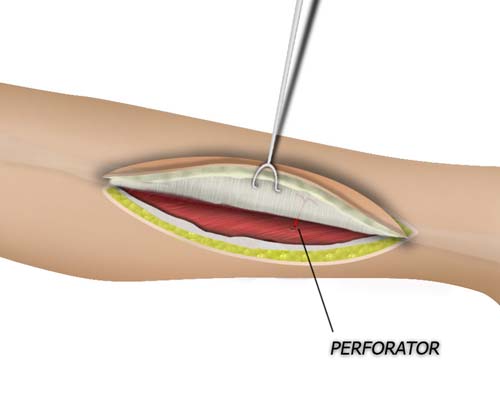
The anterior flap is elevated just above the muscle and deep to the muscular fascia. The septum is approached by elevating the fascia from anterior to posterior. Septal perforators can usually be seen from this anterior approach. If no perforators are visible, muscular perforators near the septum posteriorly must be preserved and harvested in a perforator flap fashion to the posterior tibial vessels to preserve skin paddle viability. This requires dissection through the anterior aspect of the soleus muscle.
The skin paddle is raised from the posterior approach noting and preserving muscular perforators if adequate septal perforators were not visible from the anterior approach.. If septal perforators were present, the muscular perforators are ligated and the septal vessels are preserved.. Attention is then turned to the fibula bone.
A small cuff of muscle - a millimeter or less - is left attached to the fibular bone as the surgeon proceeds medially from the anterior approach. Army-Navy retractors help provide countertraction as the muscle is peeled away leaving behind a cuff of muscle overlying periosteum on bone. The dissection is tedious to the unfamiliar, but relatively quick for the experience surgeon since it is essentially just a sharp transection of attached muscle.
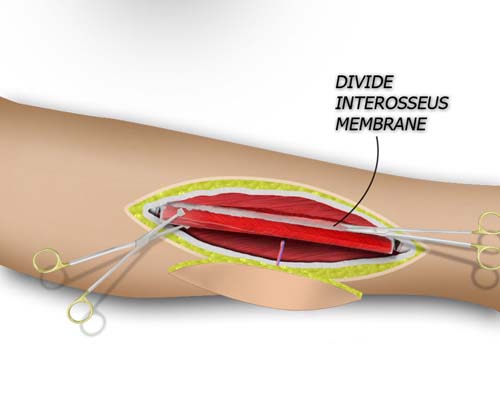
The proximal and distal fibula osteotomies are made and then a bone clamp is used to retract the fibula and expose the interosseus membrane. The mebrane is divided sharply and the peroneal vessels become exposed immediately below the membrane.
When the superior and inferior locations of the planned osteotomy are marked, a right angle retractor is is used to to snugly encircle the bone. Care is taken to hug the bone so that the vessels are not captured. The distal 6-7 centimeters if bone are preserved to spare the ankle mortise and the proximal course of the peroneal nerve is marked at the neck of the fibula to spare the nerve. This usually still leaves behind a significant length of bone that varies in size with the patient height and build. Ribbon or Homan retractors are used to protect the soft tissue when the osteotomy is made with an oscillating or giggly saw. Bone clamps can then be placed at the superior and inferior ends of the flap to help provide anterior and posterior traction on the interosseous membrane. The interosseus membrane is divided, the peroneal artery and the accompanying venae can then be seen. The distal aspect of the artery and veins are ligated and divided, and the flap can then be raised superiorly on the vascular pedicle. The tourniquet can then be deflated to obtain hemostasis and ensure good blood flow to the foot.
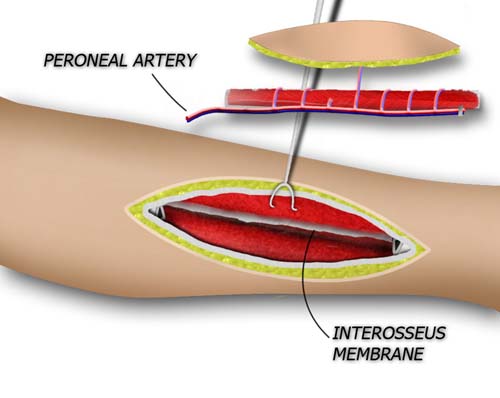
Proximal and distal osteotomies are performed, hugging the fibula subperiosteally for protection agains injuring the vascular pedicle. Bone clamps can then be placed on the fibula and it can be retracted posteriorly while the interosseous membrane is transected sharply in a longitudinal fashion.
Post-Operative Care
The ankle is splinted in neutral and the patient is allowed to ambulate in a cast shoe at about a week after surgery, usually with an ace wrap to prevent edema. At all other times the foot is kept elevated. The donor site can heal slowly if closed under tension or in the elderly patient.