Medial Gastrocnemius Muscle Flap
Anatomic considerations
The medial gastrocnemius muscle flap is not usually harvested as a free flap. However, it can be. And in addition microsurgical techniques can greatly enhance the mobility and length of the flap when used locally. Rather than a distant free flap, it can be used as a local free flap.
In our practice, we rarely use a pedicled medial gastroc. The donor defect causes an unsightly deformity, which is especially unpleasant to younger patients. The contour depression that results from medial gastroc rotation can be significant. And younger patients that comprise much of the lower extremity trauma population dislike the increase in local scarring. However, there are rare indications in our practice. If the medial gastroc cannot reach the recipient defect without excessive tension, or if the dead space cannot be obliterated adequately, the leash of the flap can be extended with microvascular surgery. The vein length can be augmented microsurgically on the lesser saphenous vein, and the artery can be grafted with the distal lesser saphenous vein as an interposition graft.
Vascular Anatomy
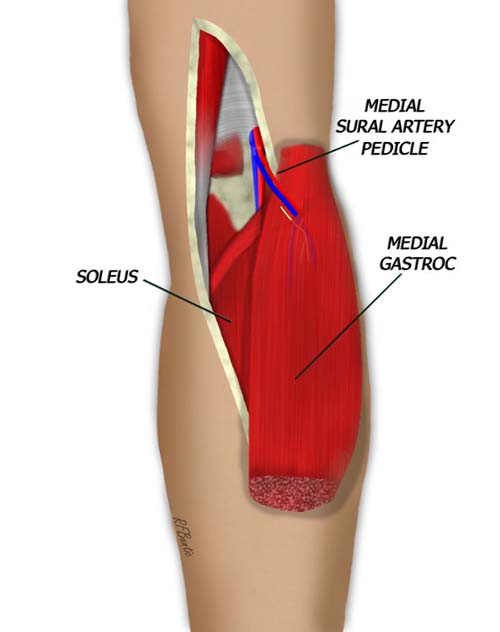
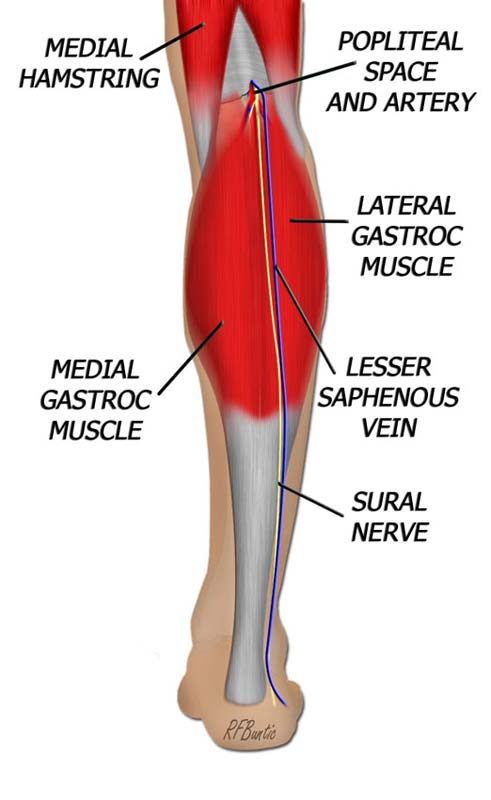
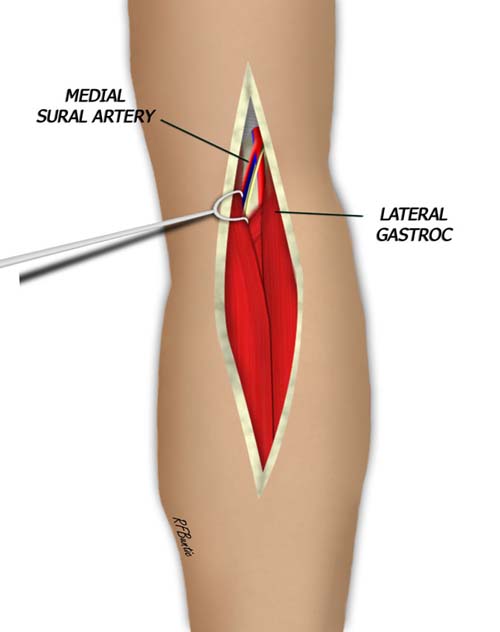
The medial and lateral gastrocnemius muscles each have independent vascular supplies. The medial muscle is nourished by the medial sural artery, while the lateral is supplied by the lateral sural. Both vessels take origin from the popliteal artery. The nerve supply is also independent, with branches from the tibial nerve going to the medial and lateral gastroc independently.
Vascular anatomy of the gastrocnemius muscle. The medial gastrocnemius is supplied by the medial sural artery, a branch of the popliteal artery.
The Operative Procedure
The patient can be placed prone, but if an anterior wound is being resurfaced, the supine position with frog leg abduction and a bent knee is used. A thigh tourniquet may be used, depending on surgeon preference.
The longitudinal raphe of the gastroc that separates medial and lateral muscle can be palpated in the popliteal fossa to orient the incision. The incision starts in the medial aspect of the fossa, over the lateral origin of the medial gastroc. A lazy "S" descends parallel to the midline of the muscle inferiorly.
As the subcutaneous tissue is entered the lesser saphenous vein is encountered and preserved by retracting it laterally. Deeper, the sural nerve is encountered and also spared.
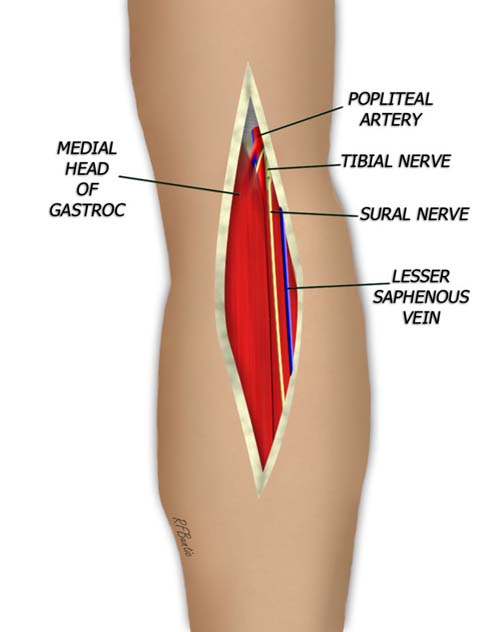
The sural nerve and lesser saphenous vein are encountered while dissecting to the muscular fascia. The deep fascia is divided and the popliteal space is entered. By identifying the popliteal vessels, the branches to the gastrocnemius can easily be identified.
Between the two proximal heads of the muscle, the pedicle to the medial gastroc is identified and traced under the muscle. The nerve branch to the medial gastroc is also identified.
The branch to the medial gastroc can be traced under the muscle and the entrance of the pedicle into the muscle can be identified.
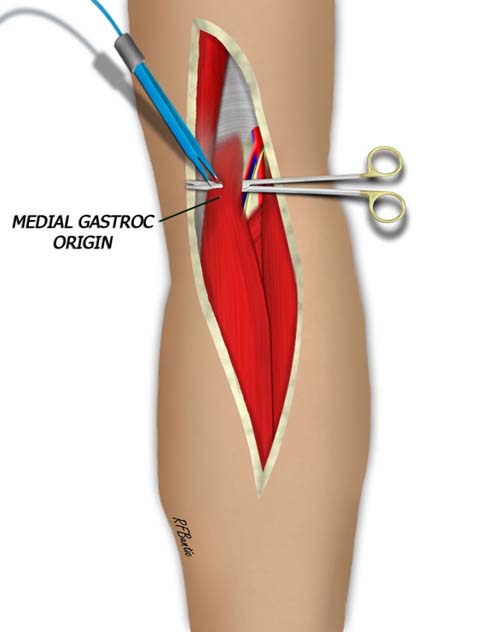
The very proximal aspect of the muscle, proximal to the pedicle is then encircled with a finger, scissors or hemostat. The origin of the muscle can then be divided.
In a similar fashion, the distal muscle is dissected free, splitting the muscle from the lateral gastroc. The plane here is not areolar and must be dissected sharply if under tourniquet control or with bipolar electrocautery. When the distal musculotendinous junction of the medial gastroc is identified, the muscle can be transected distally. The muscle is then isolated on the pedicle.