The superficial circumflex iliac artery (Groin) flap
Anatomic considerations
Vascular Anatomy
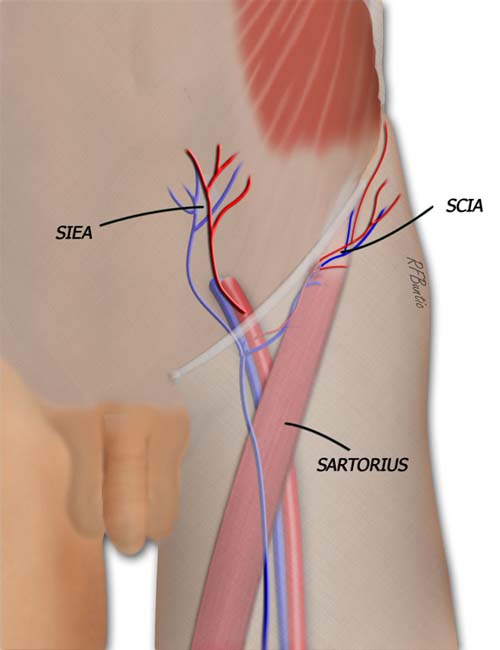
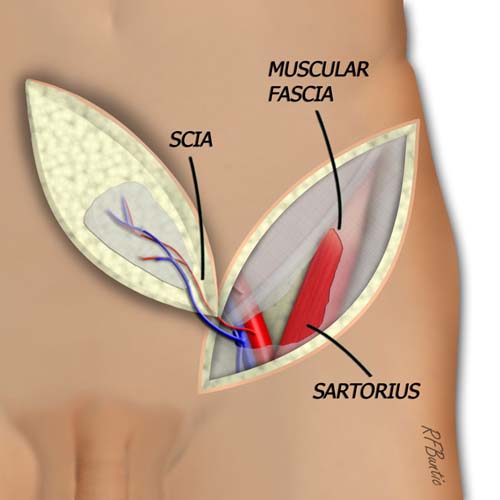
The groin flap is supplied by the superficial circumflex iliac artery system. The artery takes origin from the superficial femoral artery and the vein drains into the saphenous system. The sartorius muscle muscle provides a landmark for finding the pedicle to the flap.
The arterial inflow to the groin flap is provided by the superficial circumflex iliac artery (SCIA), a branch off the external iliac/superficial femoral artery at the level of the inguinal ligament. Venous drainage is provided by a cutaneous vein that drains into the saphenous system below the inguinal ligament. The SCIA pierces the fascia at the medial aspect of the Sartorius muscle, making the Sartorius a key landmark in identifying the pedicle during dissection.
Operative Procedure
The patient is placed supine. If a long flap is expected, a well padded bump can be placed under the ipsilateral hip to help ease exposure of the lateral aspect of the flap. The sartorius muscle, inguinal ligament, and iliac crest are all identified and marked to determine flap design. A pencil Doppler is used to determine the location of the arterial pedicle, usually approximately a finger breadth below the inguinal ligament. The maximum width of the design is determined by pinching the skin to assess the potential tension of the closure after flap harvest.
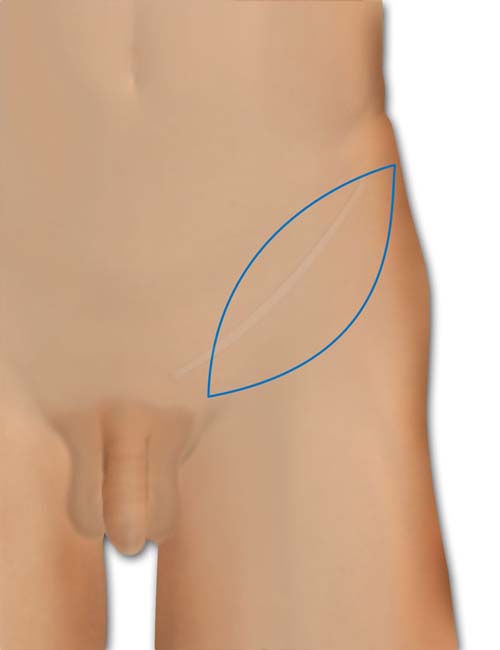
The axis of the flap is a finger breadth below the inguinal ligament. A pencil Doppler can be used to define the distal course of the artery.
The flap dissection can be begun medially or laterally. Our preference is to make the superior incision and elevate from the distal superior aspect toward the medial origin of the flap. The incision is carried down to the deep fascia and the dissection begun over the deep fascia, identifying and ligating perforating vessels as one proceeds medially.
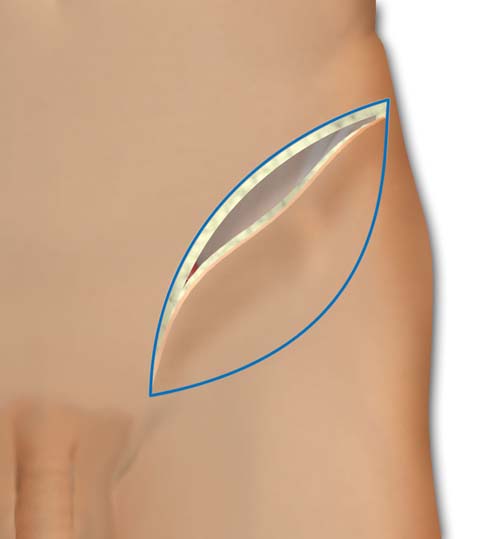
The superior and medial incision is made down to the level of the muscular fascia and the flap is then elevated from lateral to medial.
At the level of the anterior superior iliac spine (ASIS), the interval between the tensor fascia lata and the sartorius muscle can is identified. In addition, the lateral femoral cutaneous nerve of the thigh is identified as it exits the deep fascia to enter the subcutaneous tissue in its inferior course. Depending on the course of the nerve, it may need to be transected.
The Sartorius muscle is a key landmark in dissection. When the lateral aspect of the muscle is identified, the muscular fascia is incised along the lateral aspect, and the flap elevation plane is now conducted deep to the muscular fascia. Proceeding medially, the superficial circumflex iliac vessels become visible in the plane above the Sartorius heading into the muscular fascia. As the dissection proceeds, the skin incisions can be continued inferiorly and medially to relieve tension and without fear of transecting the pedicle.
Any branches to the muscle are ligated. At the medial aspect of the Sartorius, the fascial plane around the pedicle is incised and the artery and vein are dissected free to their origin.
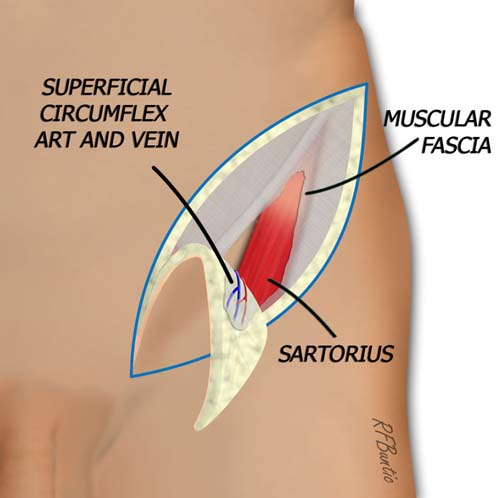
When the fascia over sartorius muscle is identified, it is incised and entered. The dissection proceeds medially deep to this fascial layer, elevating the pedicle from lateral to medial.
The flap is mobilized on the vascular pedicle. The artery may arise directly from the femoral vessel or from the trunk of a parent vessel supplying the SCIA and the DCIA. The artery can also arise from a common trunk that gives off the SIEA. The vein will arise from the saphenous vein or from a branch off the superficial femoral vein.
When the origin of the artery and vein are identified, the flap is isolated on the vascular pedicle.
The donor area is closed after slight undermining superficial to the deep fascia. A layered closure over suction drains may need to be augmented with slight hip flexion if excessive tension is present. The hip can be extended over the course of a few days.