The Parascapular Flap
Anatomic considerations
The parascapular flap provides a fasciocutaneous flap with similar characteristics to those of the scapular flap. The flap can be larger in width than the scapular flap, approaching 15 cm and has been harvested as long as 25 cm.
The anatomy of the parascapular flap allows it to be harvested with a large number of other flaps on a single pedicle, allowing for complex and large reconstructions of composite tissue defects. The parascapular flap can be combined with any one of these tissues on the subscapular vessel axis:
- Scapular flap
- Scapular bone
- Latissimus muscle
- Serratus muscle
- Serratus with rib
Anatomy
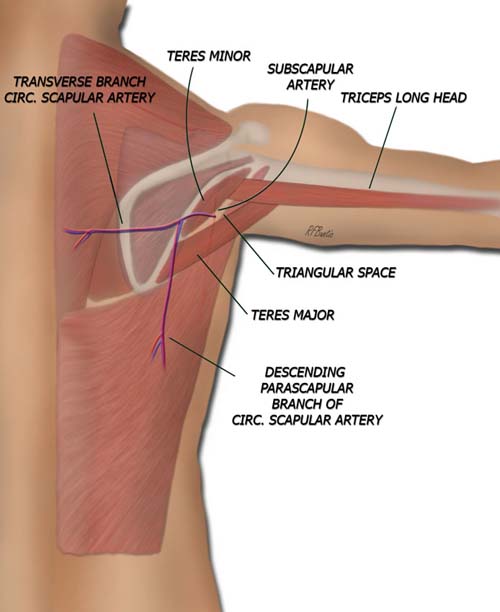
The posterior view reveals the muscles of the back. The deltoid muscle has been removed for clarity. The superior aspect of the flap is centered over the triangular space, where the circumflex scapular artery nourishes the parascapular flap after it travels through the triangular space. The borders of the triangular space are made up of the
- Teres minor
- Teres major
- Long head of triceps
The latissimus and teres major muscles are important landmarks since flap dissection proceeds from inferior to superior and these are identified early in the dissection. The elevation of the flap is performed in the areolar fascial layer just above the thick muscular fascia of the back. The infraspinous fascia overlying the infraspinatus muscle and the teres minor fascia overlying the teres minor are particularly thick. If the flap is elevated deep to the this muscular fascia, the dissection can become confusing and especially difficult around the pedicle where the fascia surrounds the triangular space.
The circumflex scapular artery is a branch of the subscapular artery which takes origin off the axillary artery. The circumflex scapular arises about 1 to 4 centimeters from the origin of the subscapular artery, but can on occasion arise directly from the axillary artery. After the circumflex scapular artery pierces the triangular space it sprouts a transverse cutaneous scapular branch and a vertical parascapular branch. The parascapular branch forms the basis of the parascapular flap.
The subscapular artery pedicle can be from 3 to 7 cm in length with vessel circumference at this level up to 4 millimeters in size. Although the circumflex scapular artery is usually accompanied by two venae commitans, the subscapular artery is typically accompanied by one vein.
Flap Dissection
The patient is placed in the lateral decubitus position on a beanbag. Optionally, the prone position can be used if a posterior wound must be resurfaced. The prone position can be technically more difficult since arm positioning can not be adjusted as easily as in the lateral decubitus position and the axilla is more difficult to dissect. The ipsilateral arm is left free and included in the operative scrub. A stockinet around the arm and Mayo stand with a well-padded pillow helps to rest the arm during surgery when the lateral position is used.
The incision is marked using the scapula as a guide. The superior flap includes the triangular space within its border so the pedicle vessel is captured in the flap. A point roughly one finger breadth below the mid point of the scapula on its lateral aspect marks the triangular space. A pencil Doppler probe can help confirm the pedicle location.
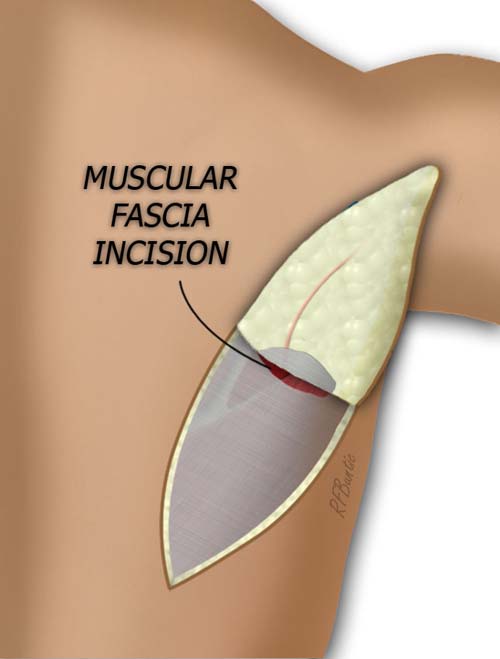
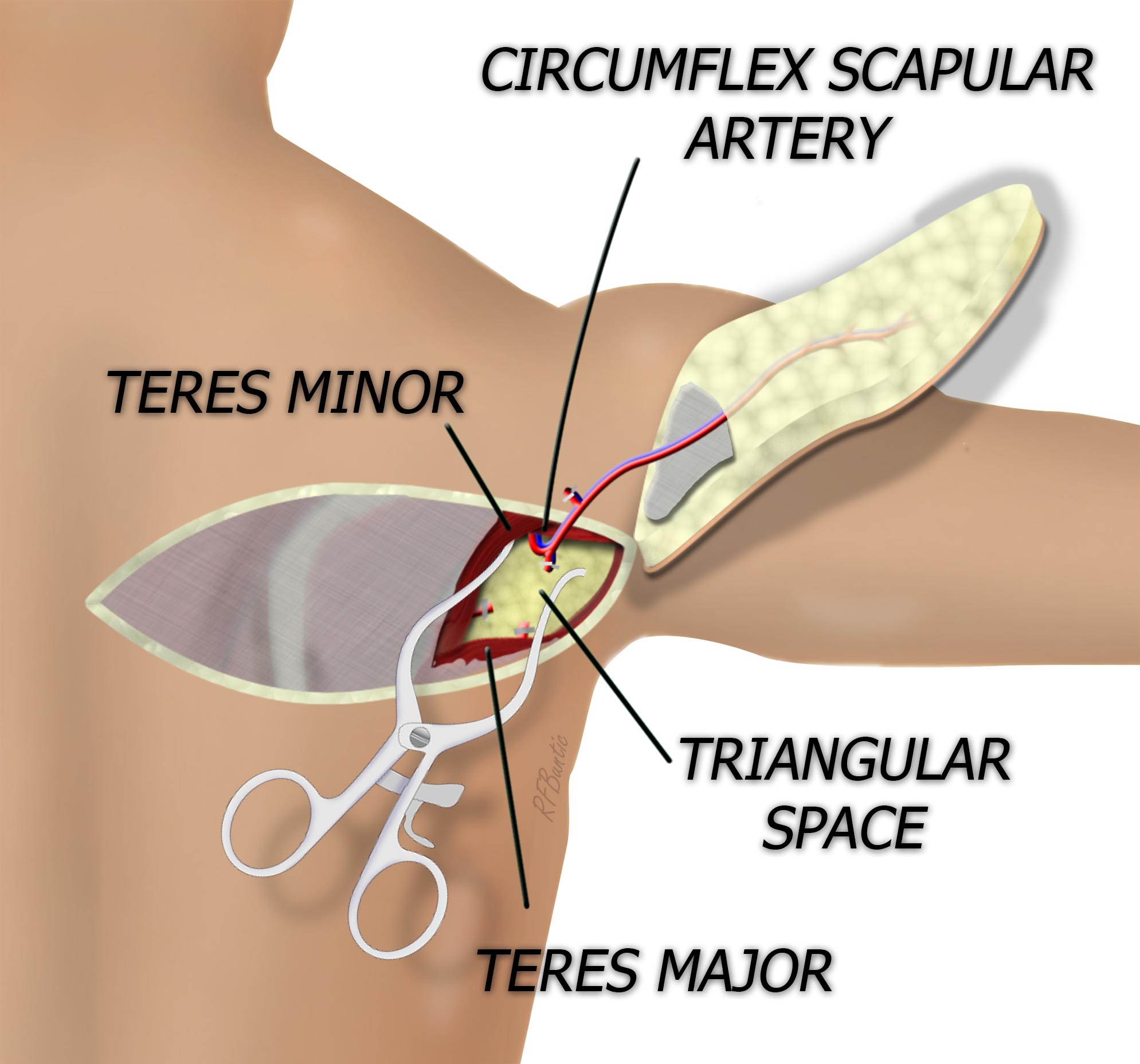
The flap is elevated from inferior to superior, superficial to the deep muscular fascia until the triangular space is approached. As the fascia adjacent to the triangular space is reached, the fascia is entered and elevated with the flap. This point is identified by a thickening of the flap with a more sturdy attachment to the subcutaneous fat, and often the vascular pedicle become visible as it pierces the fascia.
The flap is elevated from inferior to superior. The elevation of the flap is performed in the areolar fascial layer just above the thick muscular fascia of the back. The infraspinous fascia overlying the infraspinatus muscle and the teres major fascia overlying the teres major are particularly thick. If the flap is elevated deep to the this muscular fascia, the dissection can become confusing and especially difficult around the pedicle. In the medial incision the transverse arterial branch can be visualized. It is ligated before continuing flap isolation to the pedicle.
As the triangular space is identified and the pedicle traced into the triangular space, self retaining retractors and adjusting the right arm position to maximize exposure are helpful. Numerous branches must be isolated and ligated at this level before the flap is traced to the circumflex scapular artery and if needed the subscapular artery. A counter incision in the axilla can be helpful to expose and dissect the subscapular system.