Thoracodorsal Artery Perforator Flap (TAP Flap)
Anatomic considerations
Authored by Thomas E. J. Hayakawa, MD, FRCS(C)
The thoracodorsal artery perforator or TAP flap is a fasciocutaneous flap based on a musculocutaneous perforator or perforators from the thoracodorsal vessel axis and/or its vertical branch derivative. In contrast to the other well-known DIEP (deep inferior epigastric perforator) and SGAP (superior gluteal artery perforator) flaps that provide bulk, the TAP flap provides a relatively thin and pliable skin paddle. In a reasonably thin person, the flap ranges from 1 – 2 cm in thickness. In heavier patients the flap may be thinned by delaminating the deep adipose layer from the superficial adipose layer at the level of the superficial fascia. The resulting thickness of the skin and superficial fat layer will be approximately 1 cm. The TAP flap is well suited for extremity, head and neck, and peri-articular resurfacing as well as for the contouring of shallow defects. As is the case with other perforator flaps, the surgical dissection can be difficult.
A flap of dimensions 15 X 8 cm can be harvested on a single perforator. These dimensions allow for both primary closure of the donor site and avoidance of post-operative venous congestion in the flap.
Anatomy
After originating from the subscapular axis, the thoracodorsal vessels course toward the latissimus dorsi. On reaching the deep surface of the muscle, the thoracodorsal vessels most commonly divide into two primary muscular branches: the transverse branch, and the lateral or vertical branch. These branches usually diverge at near 45 degree angles to one another. Both travel from the deep surface of the muscle to become intramuscular. The lateral branch courses vertically and at least 2 - 3 cm inside the lateral border of the latissimus, often greater. A perforator or combination of perforators off the distal main thoracodorsal and/or it's lateral branch constitute the vascular supply of the TAP flap.
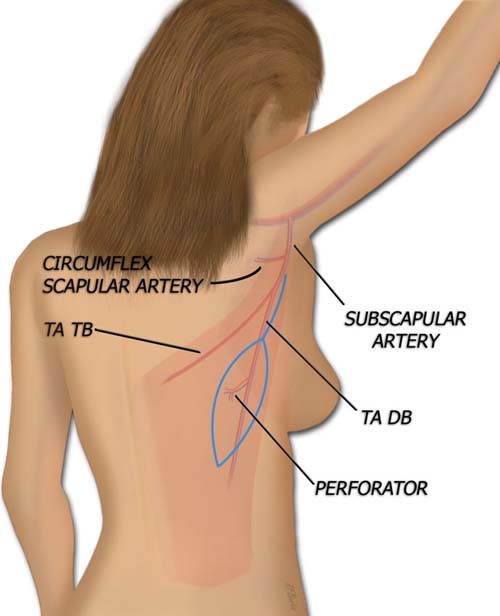
The TAP flap is nourished by perforators of the descending branch of the thoracodorsal artery.
TA TB: Thoracodorsal artery transverse branch.
TA DB: Thoracodorsal artery descending branch.
The first perforator is located approximately 6 – 8 cm below the posterior axillary fold and may be either a branch of the distal main thoracodorsal or arise from it's lateral branch. Subsequent perforators, up to a total of three, arise at 1.5 – 4 cm intervals inferiorly off the lateral branch. Each perforator displays a 3 – 5 cm oblique course through the substance of the muscle giving off numerous muscular branches before penetrating through the dorsal thoracic fascia to supply the overlying skin and subcutaneous fat layers. Each perforating artery is 0.3 - 0.6 mm in diameter and accompanied by two venae commitans.
Operative Technique
The patient is placed in the lateral decubitus position on a beanbag just as in the latissimus harvest. The ipsilateral arm is left free and included in the operative scrub. A stockinette around the arm and Mayo stand with a well-padded pillow helps to rest and optimally position the arm during surgery.
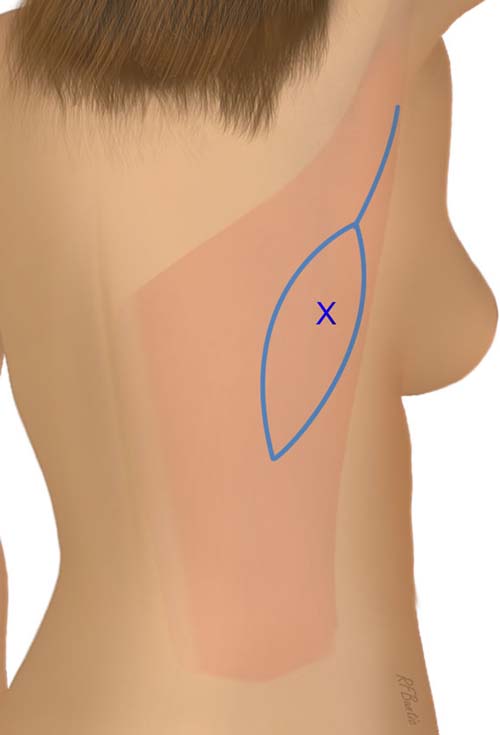
The lateral border of the latissimus is palpably identified and outlined with a marking pen. A pencil Doppler is used to identify and map out the perforators starting about 6 – 8 cm below the posterior axillary fold and 2 – 4 cm inside the lateral border of the latissimus. The loudest one to two perforators are marked.

The main perforator(s) are identified with a pencil Doppler probe, posterior to the anterior border of the latissimus muscle.
The flap dimensions needed are outline, with the perforator on the longitudinal axis of the flap. The perforator can be at the center, distal or proximal aspect of the flap, depending on the needed orientation in the recipient area. This results in an ellipse with its anterior longitudinal arc skirting the lateral border of the latissimus. The maximal width is determined by the pinch test to determine what can be closed primarily. The maximum reliable length of a TAP flap that can be elevated on a single perforator has not been clearly established. Flaps up to 25 cm in length have been reported.
The anterior or posterior incision can be made first. If you are unsure of your marking, the anterior exposure may be simpler to start with. The perforator(s) are identified. The dominant perforator is traced through the muscle to the descending branch of the thoracodorsal artery. A cutaneous nerve may be seen accompanying the largest perforator. A second perforator that appears to be in the same longitudinal plane as the first can also be dissected free and used to further nourish the flap (not pictured).
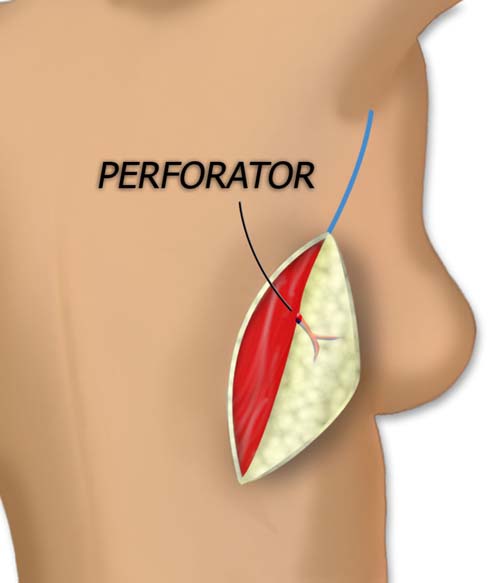
The flap is elevated medial to lateral or lateral to medial, and the perforator through the latissimus muscle to the overlying skin and fat is identified.
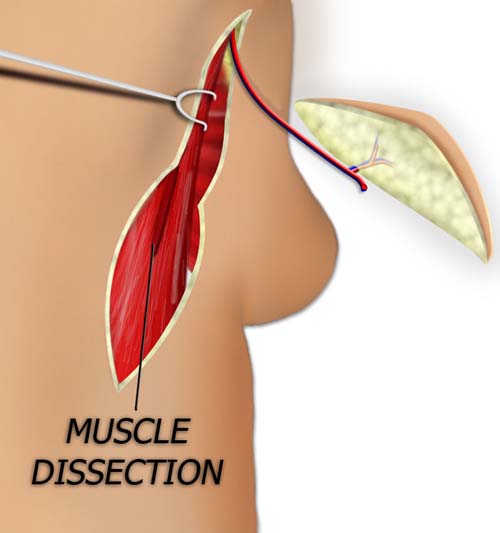
The perforator or perforators and the lateral branch of the thoracodorsal vessels are traced proximally until the deep surface of the muscle is found and the plane between the latissimus and serratus is entered. The latissimus muscle can then be retracted posteriorly with further dissection done in this plane. Bipolar cautery is used to ligate the multiple small muscular branches that are present during all stages of the dissection.
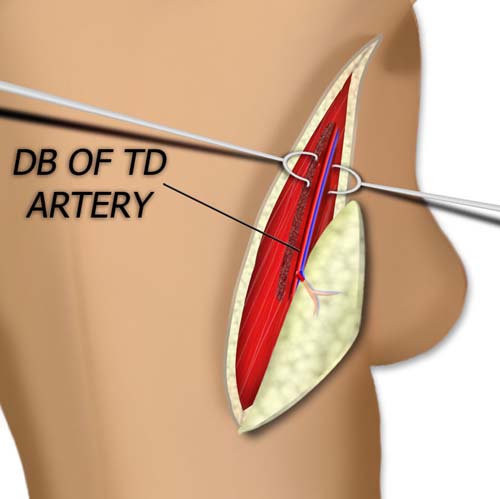
The perforator is traced through the muscle and the artery is followed toward the axilla and the thoracodorsal system.
The vessels distal to the perforator are clipped after care is taken to separate the accompanying thoracodorsal nerve. The proximal vessels are also separated from the nerve and the desired length of thoracodorsal pedicle liberated. The vessels are ligated, and with gentle traction on the flap are simply pulled through the split in the muscle.
For maximal length and vessel caliber, the artery can be followed to subscapular origin on the axillary vessels.
If adequate pedicle length and vessel diameter are present, the pedicle may be divided here. If a longer pedicle with larger diameter vessels is necessary, the transverse branch of the thoracodorsal is ligated and dissection proceeds up the main thoracodorsal axis as required. Distally, the perforator becomes so small that separating the nerve at this level could prove disastrous. Therefore, at some point, the distal intramuscular branches of the thoracodorsal nerve accompanying the perforator must be sacrificed and left adherent to the pedicle. This trivial amount of denervation is surely inconsequential. If there is a desire to neurotize the flap the previously mentioned cutaneous nerve can be separated off the main nerve branches proximally by intrafascicular dissection.
The edges of the vertical muscle split are approximated with absorbable suture. Closure of the back wound proceeds in the usual fashion. Suction drains are placed and the patient is allowed to move the ipsilateral arm post-operatively.