Facial Reanimation for Cranial Nerve VII Palsy/Paralysis
Facial paralysis can result from multiple causes, most commonly from trauma, congenital malformation, tumor resection or Bell's palsy. Early diagnosis is important, to rule out correctable causes and to act before facial muscle degeneration. In children, elective reconstruction can be considered after 2 years of age. The extent of paralysis, and patient history combined with clinical examination dictate the choice of treatment.
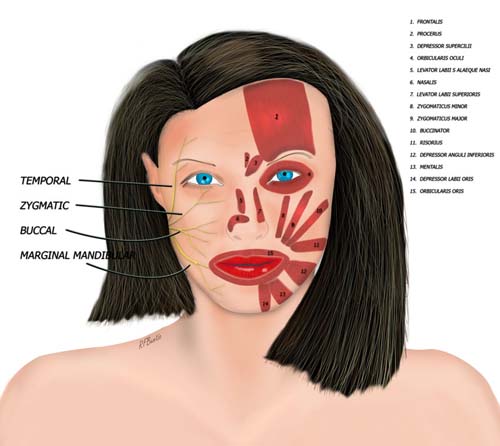
Anatomic arrangement of the facial nerve and muscles. For clarity, the nerve is depicted on the right side of the face and the facial muscles on the left.
The facial muscles work to move the forehead, eyes, face, upper lip, mouth and lower lip. The illustration divides the face in half and shows the facial muscles on the woman's left side and the branches of the facial nerve on the other. Pictured below are the temporalis and mandible muscles, which strictly speaking are not muscles of facial expression, but muscles of mastication. The medial and lateral pterygoid, which aid in the lateral movement of the mandible, are also muscles of mastication and are not pictured (they are set deep in the mouth, posterior to the palate). The buccinator is sometimes considered a muscle of mastication as well (it is pictured in the figure above), since it helps to push food from the lateral mouth to position food in between the teeth for chewing. The main muscles of mastication (temporalis, masseter, medial and lateral pterygoids) are not supplied by the facial nerve, but by the trigeminal nerve. As a result, the are not affected by facial nerve palsy.

The temporalis and masseter muscles are muscles of mastication. The other two muscles of mastication, the medial pterygoid and lateral pterygoid are not pictured.
Surgical Treatment
The surgical treatment of facial nerve injury can be divided into the following groups:
- Facial nerve repair
- Facial nerve repair with nerve grafting
- Hypoglossal nerve transfer
- Local (regional) muscle transfer: temporalis and masseter muscle transfers
- Microvascular functional muscle transplantation
A thorough history and physical examination are performed to determine the duration of paralysis, the location of the lesion, the cause of the paralysis and the degree of the paralysis. The patient with a facial paralysis is evaluated by observation in both the resting and active phases of facial expression, with attention paid to movement during speech, smiling, laughing and sometimes with ingesting food. Facial muscle functions can be variably affected depending on the extent of facial nerve paralysis. Paralysis of the nerve can affect the brow, eye, nose, mouth, lower lip - depending on the branches of the facial nerve affected (see illustration above). The eyelids and eye closure as well as the blink reflex are examined. If the patient is able to move the lips in a downward direction, depressor muscle function and platysma muscle function are present. If hearing or taste are affected or decreased tear production is present in the eye, then the facial nerve is injured in the intra temporal course where it gives off branches involved in hearing and taste.
Surgical reconstruction depends on both the extent of the injury and the level of the injury. Lesions involving transection of the facial nerve in the extra temporal course are repaired primarily if adequate nerve is present proximally and distally. If proximal and distal nerve ends cannot be repaired, but are present, then nerve grafting is performed. If a proximal nerve stump is not present, then a nerve transfer from the hypoglossal nerve or a cross facial nerve graft can be considered. If the time after injury is great, and the facial muscles have been denervated for a long time, then local muscle transfers or a functional muscle transplantation can be an option. Local muscle transfers (temporalis tendon transfer, masseter muscle transfer) have generally been discarded from the modern microsurgical armamentarium. Functional muscle transplantation has in most cases become the standard treatment for congenital and long standing facial paralysis.
In functional muscle transplantation a branch of the opposite facial nerve is used together with a cross facial nerve graft to supply a motor to a muscle transplant on the affected side. The gracilis muscle is typically utilized, although the serratus muscle or partial latissimus can be used as well. Our preference has become the gracilis muscle because of the segmental innervation, consistent anatomy and inconspicuous donor scarring.
In unilateral paralysis a two stage operation is used. In bilateral paralysis, reconstruction can be performed in a single stage with a different strategy than we use in unilateral palsy. In these cases, the motor branch of the trigeminal nerve is used for motor reinnervation.
The Two Stage operation
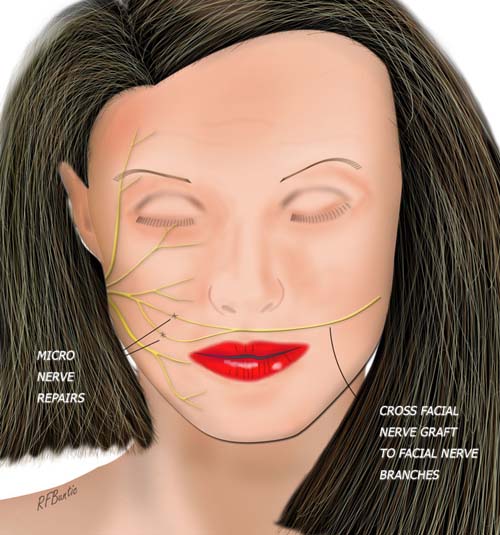
Stage One Cross Facial Nerve Grafting
Branches of the non-parlalyzed facial nerve are exposed and used as donors to motor the cross facial nerve graft. The graft is microsurgically repaired to distal functioning nerve branches, allowing re population of the nerve graft with sprouting axons used to innervate a functional muscle in 6 months to a year after the first stage operation.
We work with two teams, a surgeon and assistant on the face and a second surgeon and assistant harvesting the nerve grafts from the leg.
The patient is positioned supine, as in a rhytidectomy. The nasotracheal tube should be fixed to the forehead or the chin, leaving the upper lip free for the subcutaneous tunnel enclosing the nerve graft.
The skin incision is a modified face lift type. Instead of curving in a retroauricular fashion, inferior to the tragus the incision extends sub mentally, a finger breadth below the body of the mandible.
The cervicofacial flap is raised to expose the area overlying the zygomatic and buccal branches of the facial nerve at the anterior aspect of the parotid gland.
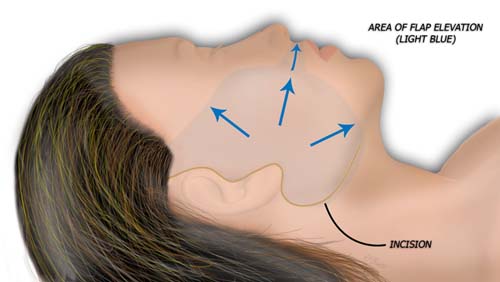
A cervicofacial flap is elevated to expose the distal branches of the facial nerve, for preparation of the cross facial nerve graft.
Distal donor nerve branches are identified by dissecting them free under loupe magnification. Their innervation is determined with a nerve stimulator. The multiple branches of the distal facial nerve allow for two or three branches to be donated without any significant paralysis resulting.
The donor nerve team simultaneously harvests the superficial peroneal or sural nerve in either the ipsilateral or contralateral leg.
A contralateral cervicofacial flap is elevated on the paralyzed side to receive the nerve graft ending.
The nerve graft is passed from through the subcutaneous tunnel of the upper lip from the non-paralyzed to the paralyzed side, using a large red rubber catheter. The catheter lumen is moistened with saline and passage of the nerve is facilitated with suction application, taking care to secure one end of the nerve. The merits in placing the neve in the orthodromic or antidromic orientation is debatable and the answer may be dependent on the duration of paralysis.
The nerve graft is then split into two major fascicles and each major fascicle is coapted to the facial nerve donor branches on the non-paralyzed side. The repairs are typically performed to a zygomatic branch and a risorius branch
The free ending nerve on the paralyzed side of the face is left anterior to the tragus and the incisions are closed bilaterally. A face lift dressing is placed.
The growth of axons across the cross facial nerve graft is evaluated by progression of a Tinel's sign in the nerve graft. When the Tinel's sign has reached a point accessible to microsurgical nerve repair of the functional muscle transplant, then the second stage can be performed. This usually requires at least 6 to 12 months.
Second-stage: Functional Muscle Transplantation
Simultaneous gracilis muscle harvest and preparation of the paralyzed side for the face are performed by two microsurgical teams.
The previous incision on the paralyzed side of the face is used and the cervicofacial flap is elevated. The extent of the flap undermining differs because the modiolus of the orbicularis muscle must be accessible to suture to the functional muscle. The nerve graft is mobilized to the area of he preoperative Tinel's sign and it is sectioned to examine the regenerated nerve. The 'yeux d'escargot', or snails eye appearance of regenerated axons are a sign of regrowth of the nerve.
The facial artery and facial vein are identified and tagged with vessel loops in preparation for the muscle transplant. The location of the artery is found by palpation of the pulse near the central aspect of the body of the mandible.
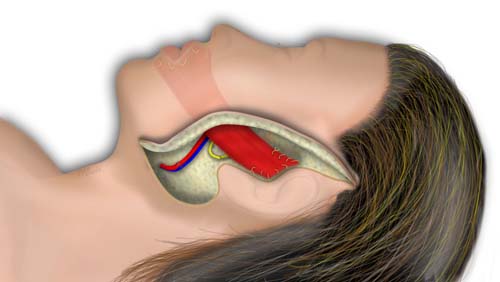
When the gracilis muscle is harvested is it brought to a side table and the nerve is micro dissected to separate the three main axon units and the innervation of these units on the muscle is mapped. The muscle is appropriately thinned with this anatomic arrangement in mind.
The muscle is then inset to the periorbital area, taking care not to injure the cross facial nerve. The lateral nose, upper lip, modiolus and lower lip are tacked to the distal muscle. The proximal muscle is then placed on tension, effectively making a static sling on the paralyzed side. Appropriate tension is kept by tacking sutures to the deep tissues around the zygomatic arch.
The artery and vein of the muscle are then microsurgically repaired to the facial artery and vein. Once blood flow to the muscle is established, the nerve to the muscle is co-apted to the cross facial nerve graft.
The cervicofacial flap is closed over a Penrose drain and a face lift dressing is placed.
Post Operative Care
Patients are monitored for hematoma formation and muscle perfusion anomalies. Discharge is usually in 4 to 5 days on a soft diet. Sutures are removed at approximately one week.