The Radial Forearm Flap
Anatomic considerations
Preoperative Assessment
The skin of the volar forearm provides relatively thin and reliable coverage for a wide variety of defects. Because the radial aspect of the arm is hair bearing, the amount and quality of the hair is a consideration in using this flap for resurfacing.
Any previous intravenous lines or arterial line placement may impact the flap vascularity and should be considered. An Allen's test can help to elucidate the continuity of the palmar arch and any potential radial sided vascular insufficiency resulting from loss of continuity of the radial artery. However, even if the Allen's test reveals an incomplete arch, the radial forearm flap can be harvested if the radial defect is reconstructed with a reverse saphenous vein or cephalic vein grafting.
Anatomy
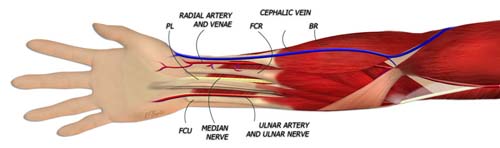
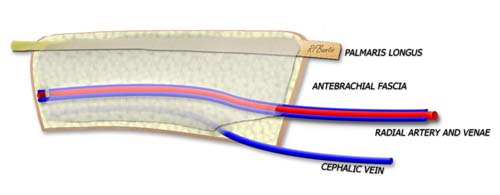
The radial forearm flap is supplied by the radial artery and perforators from the radial artery to the overlying skin. The venae commitans of the radial artery or the cephalic vein can be used for venous drainage.
The radial artery provides nutrient inflow to the flap via perforating vessels that pierce the antebrachial fascia as they course toward the subcutaneous fat and skin. The radial artery is easily palpable in the distal forearm and it's course can be marked by following the pulse proximally. Veins accompany the radial artery and the subcutaneous cephalic vein is at the radial most edge of the forearm. This large vein can be incorporated into the flap distally, or left behind to use for radial artery reconstruction after flap harvest.
Dissection
The donor arm is placed on an operating arm board abducting the shoulder at ninety degrees to the patient. A padded tourniquet is used proximally before prepping and draping. The size of the flap is determined and marked on the forearm, often with a template from the defect or estimate of the defect size. Because the flap can be folded, creative designs can be used in the harvest to reconstruct 3-dimensional defects.
The traditional flap outline has the radial most aspect over the radial artery. The flap can extend ulnarward to the less hair bearing part of the forearm as desired. If a tendon graft is needed, the palmaris longus is included in the flap. If bone is needed, a portion of the distal radius (leaving dorsal and radial cortices) can be used. The defect can be prone to fracture and this must be considered in postoperative mobilization or as a possible indication for prophylactic plating.
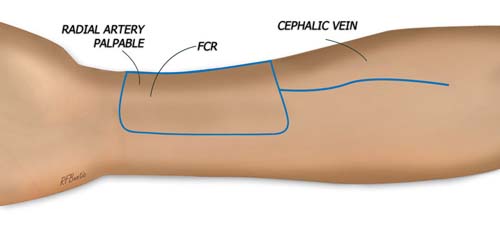
The course of the radial pulse is determine and the flap is outlined over the radial artery. The position of the flap can be pushed radially, ulnarly, or more proximally depending on the needs of the recipient area. Consideration should be given to the location of the cephalic vein if that is to be used for venous drainage.
The distal aspect of the flap is raised first. The dissection proceeds deep the the antebrachial fascia, elevating the fascia with the flap. Paratenon is left on the FCR tendon and palmaris, if the palmaris is to be left behind. The palmaris is often harvested with the flap, since it is expendable and can be used in the area of reconstruction as needed.
The radial artery and venae commitans are ligated and divided distally. The flap can then be raised from the distal aspect. As the dissection proceeds proximally, the pedicle travels under the brachioradialis tendon and muscle, necessitating retraction of this unit. Care is take to avoid injuring the dorsal branch of the radial nerve, which exits into the distal forearm from underneath the brachioradialis muscle.
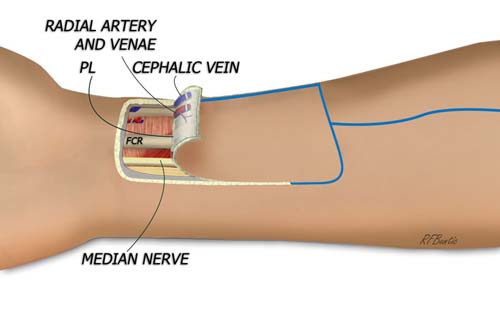
The flap is raised from distal to proximal, dissecting deep to the antebrachial fascia and ligating the radial artery and its venae.
The cephalic vein or a cutaneous vein can be taken with the flap, and we usually take one or the other. If the radial artery is to be reconstructed by a second team, the cephalic vein can be reversed and used for the reconstruction.
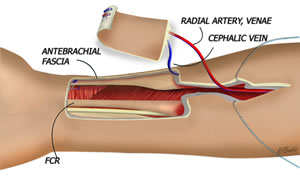
As the dissection proceeds proximally, the radial artery runs very tightly with/underneath the ulnar aspect of the brachioradialis tendon and muscle.
The defect left by the flap can be primarily closed if small, but is usually skin grafted. The patient is splinted to immobilize the wrist. The fingers are kept free.
The cephalic vein provides a separate venous leash with large caliber for approximating to large veins in the area of reconstruction.
Complex Flap Designs
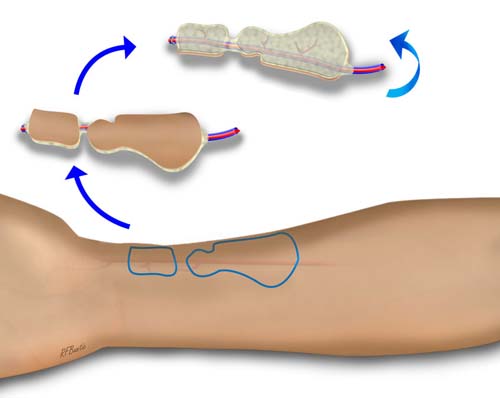
The radial forearm donor area is thin and vascular enough to allow very esoteric flap designs, with separate skin islands that allow flap folding and shaping to reconstruct complex defects.
 <
<
Complex flap design with separate skin islands and sophisticated in-situ shaping can be done with the radial forearm flap(adapted from Walton and Burget, Plast Recon Surg, 120:1171, 2007).
Flap Variations
Radial Forearm Fascia Flap: the deep fascia can be harvested without the skin paddle, creating a thin fascia only flap.
Radial Forearm Osteocutaneous Flap: a segment of the radius can be harvested with the flap, in congruity with a portion of FPL muscle. It must be a unicortical block of volar radius, and no wider than 1.5 centimeters. The radius is prone to fracture is a segment of radius is harvested.
Post-Operative Care
We allow the patient to use the donor hand as tolerated, but emphasize elevation to minimize edema and promote wound and/or skin graft healing. If donor bone is taken with the flap, stressing the radius with more than ten pounds of weight is avoided for at least six weeks. Radiographs can help to determine the extent of bone healing.