The Transverse Rectus Myocutaneous (TRAM) Flap
Anatomic considerations
Anatomy
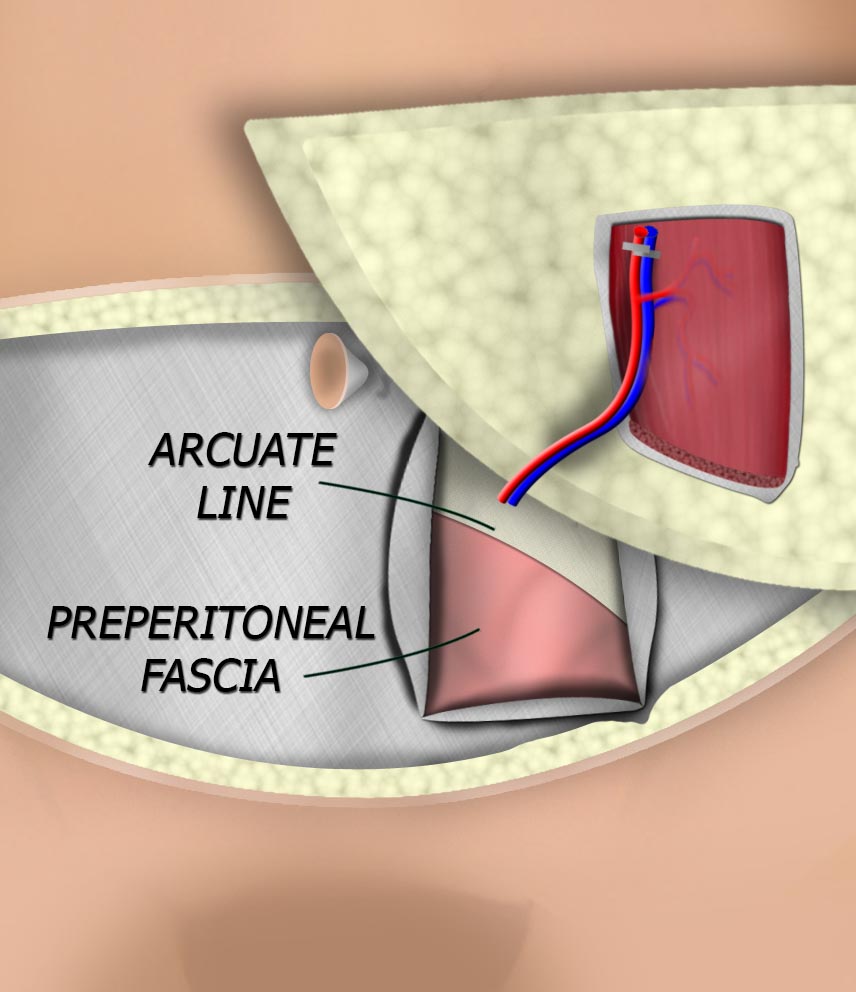
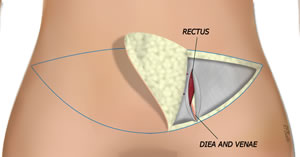
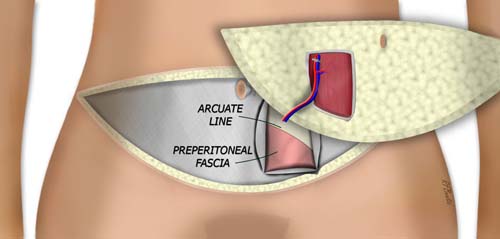
The paired rectus muscles provide abdominal flexion and support for the intra-abdominal contents. The origin of the muscles is the pubic symphysis and pubic crest, while the insertion is the fifth to seventh costal cartilages. The muscle is enclosed by the rectus sheath, but below the arcuate line, this sheath disappears posterior to the muscle. An important area of weakness that should be recognized when securing abdominal closure after flap harvest. The arterial supply to the lower muscle and overlying fat and skin is the deep inferior epigastric artery and venae. The muscle can be up to 30 cm long and up to 10 centimeters wide.
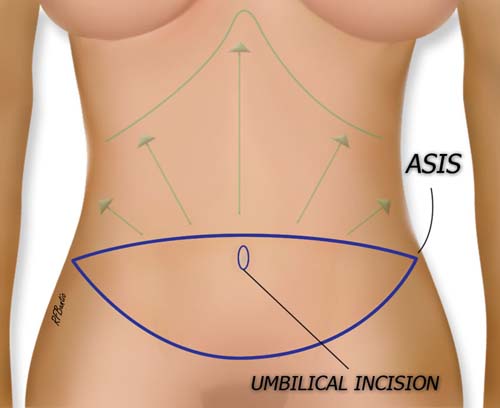
The lower abdominal skin is used in the TRAM, just as in the DIEP and SIEA flap. After the flap is removed, the abdominal skin and fat is undermined above the rectus sheath to the costal margin (green arrows and line) to allow closure of the donor defect.
The blue line outlines the incision, and the green arrows demonstrate the extent of undermining after flap harvest to close the abdominal donor area
After flap harvesting, the abdominal skin and fat above the flap is elevated to the costal margin (green arrows). The tissue plane is just superior to the rectus sheath. Medially the plane is quite fixed, but laterally it is less adherent. By beginning the elevation laterally and then focusing medially, the elevation is simpler.
Operative Procedure
The abdominal skin island is designed with the lower aspect of the incision transversely placed above the pubic bone, in line with the typical transverse Cesarean section incision. It extends laterally with a gentle curve superior to the inguinal ligament finishing adjacent to the anterior superior iliac spines. The upper incision is placed above the umbilicus and gently curves laterally to meet the lower transverse incision marking. With the patient in the supine position and the knees slightly flexed, the skin should be able to be pinched closed.
The flap is started by elevating from lateral to medial and the search for perforators is begun when the rectus sheath over the muscle is encountered. This dissection can be performed with a the electrocautery on a low setting, or with bipolar forceps and scissors.
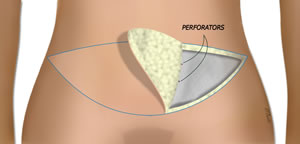
The flap is elevated superficial to the rectus fascia until major perforators over the rectus muscle are identified.
When perforators over the muscle are encountered, the fat dissection is stopped, and the fascia is incised lateral to the perforators. This represents the lateral extension of fascia that will be harvested with the flap. The DIEA vessels lateral to the rectus muscle are identified and can be traced to their origin on the external iliacs.
The rectus fascia is incised longitudinally and the to encompass the lateral extent of the major perforators.
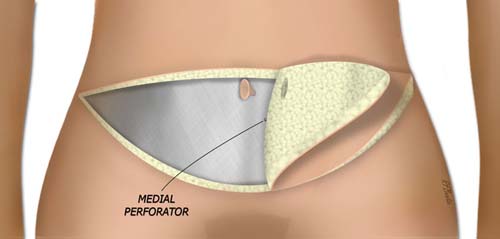
The contralateral skin flap is elevated until the most medial perforator(s) over the ipsilateral rectus muscle are encountered. The umbilicus is separated from the flap with a periumbilical incision, leaving the umbilical stalk attached to the abdominal wall.
The fascia is incised longitudinally medial to the medial perforator(s).
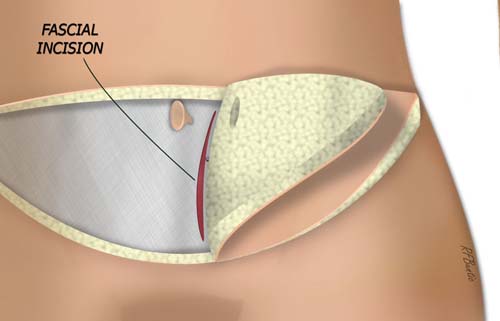
The fascia is incised medial to the medial perforators. The lateral and medial extent of fascia incision and removal are now identified.
The fascia is incised connecting the medial and lateral fascial incisions. and the rectus muscle is transversely transected at the uppermost extent of the fascial opening.
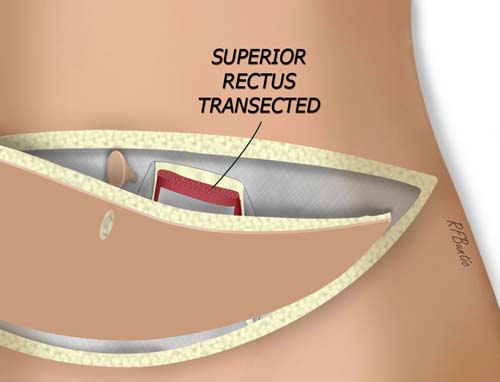
The superior fascia is incised. The upper edge of the rectus muscle can be transected and the flap can be elevated from superior to inferior.
The inferior fascial incisions are connected with a transverse entry into the fascia. The muscle inferiorly is divided, taking care to avoid injury to the DIEA vessels.
The DIEA vessels are then traced back to near their origin while retracting the muscle away from the deep abdominal contents. The entire flap is isolated on the DIEA vessel.
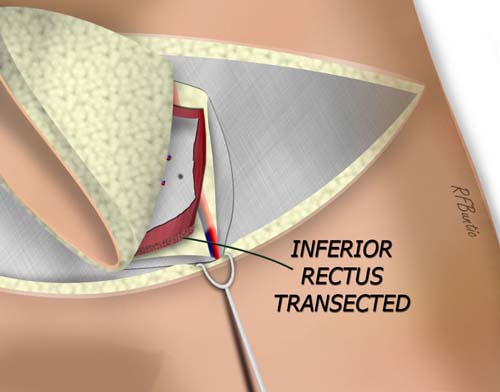
the inferior fascia is incised and the inferior muscle can be transected, taking care not the injure the deep inferior epigastric vessels.
The vessels are ligated and divided when the recipient area is ready.
the flap is isolated, leaving a fascial defect. Depending on the size of the defect, it can be repaired primarily or reinforced with mesh.
The rectus sheath is closed with a running large caliber non-braided suture, or if necessary, the fascia is closed with mesh and running suture.
The abdominal wall is undermined to the costal margin and the abdominal incision is closed in layers over suction drains with the hips flexed in a semi-Fowler position. The umbilicus is brought through the abdominal wall after it is stretched to near closure. The patient is allowed to mobilize when clinically indicated for the recipient area. The patient ambulates with the hips flexed until the tension of the closure slowly resolves.